Patient advocates want the lip smacking, grimacing and uncontrollable twitching caused by the movement disorder tardive dyskinesia to do more than attract stares.
Insurance Barriers are Parkinson's Doctors' Other Battle
Movement Disorders Patients Need Medicare's 6 Protected Classes Intact
Add movement disorders patients to the long list of people whose health could suffer under the Trump administration’s proposal to loosen Medicare protections on six classes of medications for high-risk diseases.
It's Time to Supercharge Caregiving
During National Family Caregivers Month this November, Caregiver Action Network is calling on caregivers to “supercharge” these functions through technology.
“Well Beyond Blue” Meeting Allows Patients to Voice Perspective
#CureStigma This Mental Illness Awareness Week
Will Reforming Medicare Billing Rules Benefit Patients?
How ICER Gets It Wrong
New Treatments Will Target Parkinson’s Patients’ “Off” Periods
from the Institute for Patient Access
Existing therapies help Parkinson’s patients control their tremors and stiffness – most of the time. Now, new versions of the drug apormorphine could address breakthrough symptoms, which about 90 percent of patients experience during what’s known as “off” periods.
If, that is, health plans make the drugs accessible.
Off periods typically occur after patients have been on Parkinson’s medication for five to 10 years. They manifest in one of several ways. Some patients experience a gradual wearing off of their medication before the next dose is due; or, they find the dose not taking effect as quickly as usual. For other patients, the off episode may happen suddenly.
Patients have a few different options. A simple change in routine may help; separating Parkinson’s medication from meals, for instance, because protein may block the body from absorbing the medication. Other patients may need to work with their physician to adjust the amount, frequency or formulation of their medication. A longer-acting formulation may help.
In other instances, however, patients need an additional medicine to manage off periods. Apormorphine, a rescue medication, can help by mimicking the brain’s natural dopamine. And a new formulation under review by the Food and Drug Administration makes the drug more usable for patients. While existing apormorphine is injected, the new formulation dissolves under the tongue. This could help patients who want to administer the drug themselves but are struggling with tremors or sudden stiffness.
The FDA is also considering an inhaled version of levodopa. Both therapies are expected to become available to patients in early 2019.
But the question remains: Will patients’ health plans provide access to these treatments? Innovative therapies often encounter resistance from insurers, who may use prior authorization, step therapy and high cost-sharing to minimize their spending.
Barriers like these would limit access, leaving Parkinson’s patients at the whim of breakthrough symptoms that undermine their independence. Barriers could also discourage continued innovation. Both effects could be devastating for Parkinson’s patients and their families. The estimated 1 million Americans with Parkinson’s depend upon innovative medicine to manage their day-to-day lives – and look toward the future with hope for a cure to the debilitating disease.
Teen from Broomfield wants to have a conversation with the world about Tourette Syndrome
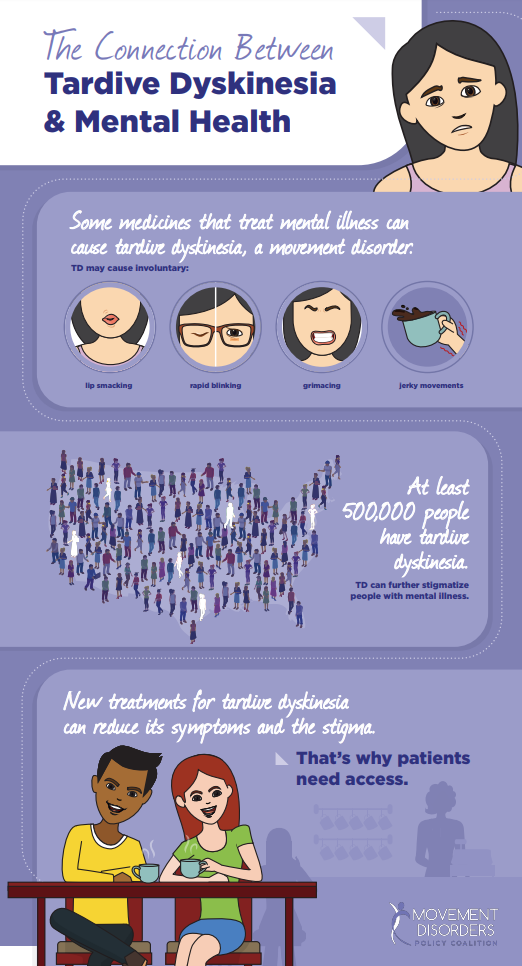
The Connection Between Tardive Dyskinesia & Mental Health
Tourette Syndrome Awareness Month: A Time to Stop the Stigma
from The Alliance for Patient Access
Many people think they know Tourette syndrome. It’s the person who blurts out foul words at inopportune times, like what you see on sitcoms or in movies. In reality, this particular vocal tic is rare. But the stereotype of people living with Tourette syndrome is unfortunately common.
Setting the record straight is important to advocates. So is raising awareness about the experiences of those who live with the nervous condition. And from May 15-June 15, National Tourette Syndrome Awareness Month, that’s the goal.
Individuals with Tourette syndrome have a combination of at least two motor tics and one vocal tic, according to the Tourette Association of America. Simple motor tics are involuntary movements like excessive blinking or shoulder shrugging, whereas complex motor tics might be twirling or jumping. Vocal tics are a sound, such as throat clearing or sniffing. Increasing public awareness about the range and type of tics exhibited by those with Tourette syndrome can help reduce the intense stigma they experience.
Yet stigma is hardly the only challenge that people with Tourette syndrome face. Access to treatment can also be difficult. Health plan barriers can complicate getting a physician-prescribed deep brain stimulation treatment or oral medication.
As the Movement Disorders Policy Coalition’s recent white paper describes, some patients face barriers to treatment because of cost-driven, health plan policies. One such hurdle is step therapy. Also called “fail first,” it requires patients to try, and fail, on a cheaper medicine before the insurer agrees to pay for what the physician prescribed. Another barrier is prior authorization. It requires doctors to gain insurance company approval before patients can begin the prescribed treatment.
Ensuring timely access to treatment along with increasing awareness and reducing stigma are all the more important because Tourette syndrome has no cure. Accomplishing these feats can improve the lives of the 1/100 school-aged children living with Tourette Syndrome or a Tic Disorder.
To learn more, read “Movement Disorders: Impact and Access to Treatment.” And join the online conversation about Tourette Syndrome Awareness Month using #TouretteAwareness.
Huntington’s Disease Patients Aim for Parity
from the Alliance for Patient Access
This month, patients with Huntington’s disease are asking for what worked for patients with ALS and other debilitating diseases–parity to accessing Medicare benefits. The request is a focal point for May’s Huntington’s Disease Awareness Month.
As Huntington’s disease advances, patients often find themselves unable to work. Accessing health insurance through an employer ceases to be an option, and buying it on their own may be unaffordable. Medicare promises stable coverage, but patients face a delay in qualifying. Currently, Huntington’s patients must have received Social Security Disability for 24 months before gaining Medicare eligibility.
The Huntington’s Disease Parity Act would remove that requirement.
Carving out an exception would eliminate the gap in treatment that Huntington’s disease patients may otherwise face. And it wouldn’t be the first time policymakers have granted an exception for patients with progressive conditions. For example, the federal government waived the prerequisite for patients with ALS, also known as Lou Gehrig’s disease. People with end-stage renal disease don’t have to wait either.
More than 30,000 Americans suffer from Huntington’s, which can cause poor coordination, involuntary movements and difficulty understanding new information. Patients are likely to experience a decline in cognitive abilities and experience more extreme mental symptoms as the disease advances.
Physical therapy, occupational therapy, speech therapy and psychotherapy help patients cope with limitations caused by the condition. Medication can treat some of the symptoms, like muscle rigidity and depression; however, there is no cure.
Until researchers make that discovery, timely access to health care is of the upmost importance. Patients with Huntington’s disease, along with their family, physicians and advocates, look to the Huntington’s Disease Parity Act to make consistent access possible.
Parkinson’s Patients Face Treatment Delays
Do you know the face of someone with essential tremor?
Living with Stigma
Living with a movement disorder means living with stigma.
Stares, whispers and pointing are just another part of the disease burden for the millions of Americans with Tourette, essential tremor, tardive dyskinesia, Huntington’s disease or other movement disorders. The stigma can have wide-range effects on a patients’ quality of life.
Tammy Dodderidge of the International Essential Tremor Foundation conveyed several patients’ experiences. “One woman described the questions she gets from her children: Why is she shaking, why grandma shakes too, or the most difficult question, the child asking ‘Will I shake like that when I grow up?’”
Another patient explained, “I have worked with the public all of my life, and you will always have people who comment on it. Most people have never heard of essential tremor …and are apologetic when they finally understand.”
But not all movement disorders patients have the opportunity to explain their condition – or want to. Some dodge awkward situations altogether by avoiding restaurants, shops and public venues. Yet social isolation can worsen the mental health challenges that many movement disorders patients already face.
Given the impact of stigma, what is the value of alleviating it?
The issue came to the forefront last year when the Institute for Clinical and Economic Review failed to account for stigma in its review of a new treatment for tardive dyskinesia. Instead, ICER simply determined that the drugs, called “VMAT2 inhibitors,” were too expensive.
“It is unfortunate that the ICER review is likely to provide payors—both public and private—with the ammunition needed to restrict access to these promising and long overdue therapies to treat TD,” noted Andrew Sperling of the National Alliance on Mental Illness.
For those with tardive dyskinesia, involuntary movements such as frowning, tongue thrusting or lip smacking can lead to social isolation. These motions can also lead to difficulty fully participating in one’s community or maintaining a job.
Ignoring one of the primary benefits of the new treatment—that it can limit uncontrollable movements and in turn, intense social stigma—is a setback for movement disorder patients.
“For patients that have been living with moderate to severe TD for years, the opportunity to finally have an innovative therapy that can allow for employment and social integration is a game changer,” Sperling added.
The movement disorders community remains hopeful about new therapies to address symptoms and alleviate stigma – and for policies that allow patients to access those therapies.
To learn more, read “Movement Disorders: Impact and Access to Treatment” from the Movement Disorders Policy Coalition.
New Law Recognizes Family Caregivers
An estimated 65 million family caregivers help their elderly, disabled or ill loved ones continue to live at home – driving them to appointments and assisting with day-to-day needs like bathing, dressing and preparing meals. Few receive recognition, resources or support. But a new law aims to change that.